Brady’s story: Finding help, balance, and hope
With his rosy cheeks, tousled hair, and outgoing personality, Brady Jorgensen of Council Bluffs, Iowa, is a poster boy for “cute kid.”
You wouldn’t guess that he’s lived with a brain tumor for most of his life.
One evening in 2007, when Brady was 9 months old, his mother, Brandy, noticed his left eye twitching. Less than two weeks later came Brady’s diagnosis.
The Pediatric Brain Tumor Clinic at University of Iowa Stead Family Children’s Hospital is the first of its kind in Iowa and one of just a few in the United States. The clinic is multidisciplinary and collaborative, which means specialists from a variety of areas come together to create a personalized treatment plan for every patient.
Families meet with all members of a child’s care team on one day, at one location, eliminating the need for scheduling several appointments with different specialists over multiple days. These coordinated discussions are focused on determining the best course of treatment for the child’s tumor.
This rare type of tumor—known as a pilomyxoid astrocytoma—often occurs in the hypothalamus, the area of the brain responsible for the body’s key hormones. It also can affect the brain’s optic nerves. For Brady, this caused the initial eye twitching, which has since led to total vision loss in his left eye and some vision loss in his right eye.
Neurosurgeons in Omaha removed 70% of the butterfly-shaped mass, but within weeks most of the tumor came back. At 10 months old, Brady began an 18-month chemotherapy regimen. When the tumor started growing in June 2010, he underwent another 13 months of chemo. In July 2013, the tumor started growing again, bringing more uncertainty to Brady’s family.
By October 2014, when scans showed that the tumor had not diminished, Brandy contacted pediatric cancer specialists at University of Iowa Stead Family Children’s Hospital, who were in the process of launching a new clinic for patients like Brady.
The Pediatric Brain Tumor Clinic at UI Stead Family Children’s Hospital, the first of its kind in Iowa, is multidisciplinary and collaborative. Bringing pediatric specialists from multiple disciplines into one clinic helps facilitate communication among providers, streamline care, and deliver a unified message to the patient and family, notes UI Stead Family Children’s Hospital pediatric neuro-oncologist Mariko Sato.
“All members of the team—from neurosurgery, neuro-oncology, radiation oncology, endocrinology, ophthalmology, neurology, and psychology, as well as social work, child life, and nursing—work together to care for patients and their families,” Sato says.

A multidisciplinary approach itself is not new. At UI Stead Family Children’s Hospital, bringing multiple specialists together to care for patients has been in place for years, says radiation oncologist John Buatti.
“What makes our Pediatric Brain Tumor Clinic unique is the formalized way we interact in a framework that not only fosters collaboration but benefits patients and families in important ways,” Buatti says.
For families, the benefit is clear: Patients typically are seen by specialists over one day at one location, eliminating the need for scheduling several appointments with different specialists over multiple days. In a rural state like Iowa, where families may travel hours to Iowa City for a clinic appointment, it’s a major convenience.
When Brady and his family arrived at UI Stead Family Children’s Hospital in January 2015, the Pediatric Brain Tumor Clinic was ready. The team had received Brady’s medical records, scans, and pathology reports from Omaha in advance and already had devised a course of treatment.
The UI team proposed fractionated stereotactic radiotherapy, which involves narrow beams of radiation administered from multiple angles to precisely target the tumor while sparing surrounding tissue. Using an advanced technology called infrared optic guidance, specialists can accurately pinpoint the radiation delivered to within tenths of a millimeter. A patient receives the radiation in small, incremental doses over time to further minimize the risk to non-cancerous areas.

Visit the UI Stead Family Children’s Hospital website to watch a three-part video series documenting Brady’s story of recovery and hope.
“They said, ‘Here’s what we can do,’” Brandy recalls. “They did their homework before we came, and they had a plan. That was comforting.”
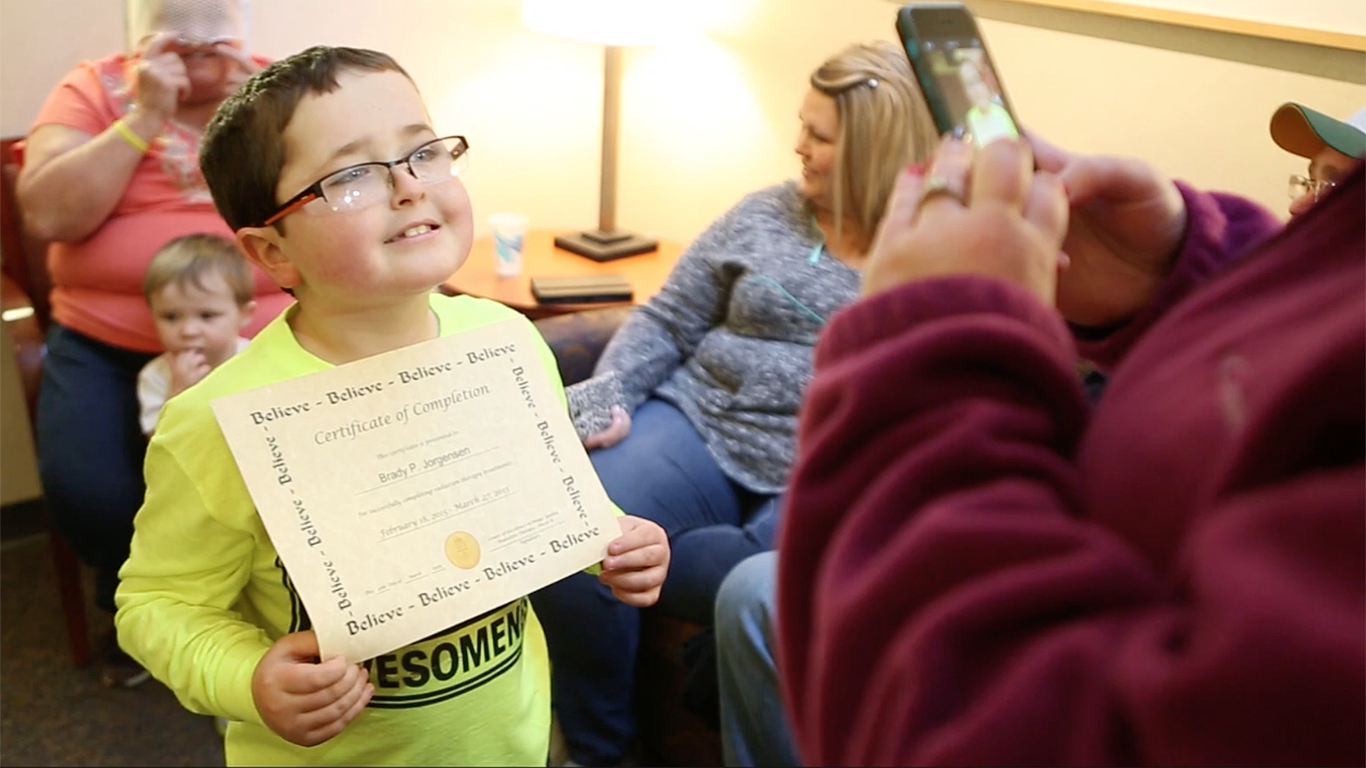
In February 2015, Brady began a six-week course of radiotherapy—28 treatments, Monday through Friday. He and his family stayed at the Ronald McDonald House in Iowa City. To keep up on his schoolwork, Brady worked every day with Megan Soliday, a pediatric teacher at UI Stead Family Children’s Hospital who coordinated Brady’s lessons with his elementary school back in Council Bluffs.
Overall, Brady’s radiotherapy sessions went smoothly. For now, the family remains cautiously optimistic. They understand this is not a cure but an opportunity for a longer and better quality of life. The UI Stead Family Children’s Hospital team will continue to follow Brady’s progress. He attends follow-up clinic appointments every four months, and the tumor appears to be well controlled.
“Brady knows this radiation is going to give him a chance,” his grandmother, Teresa, says. “And now he talks about going to college. I’m not sure we had that conversation too much before.”
For Brady, his experience at UI Stead Family Children’s Hospital has meant one thing in particular.
“Just hope,” he says. “That’s all I do is hope.”
What would Brady tell other children who have been diagnosed with a brain tumor?
“It’s going to be OK, and I have one, too,” he says. “Don’t be scared and just feel confident in yourself, and don’t back down. Don’t let it get in your way.”



