The University of Iowa welcomes another academically accomplished cohort of students this fall.
The University of Iowa continues to attract high-achieving students. This fall’s incoming first-year class has topped previous records with an average high school grade-point average (GPA) of 3.82. The average high school GPA for the incoming classes of 2021 and 2020 were 3.81 and 3.78, respectively.
It is also the third-largest incoming first-year class on record at 5,178 students, after 5,643 in the fall of 2016 and 5,241 in the fall of 2015.
“We are so excited to welcome these newest Hawkeyes, a large and accomplished class full of energy and new perspectives,” says UI President Barbara J. Wilson. “We’ll make sure they have the extraordinary opportunities they deserve as we continue to make progress on our university priorities: student, faculty, and staff success; transformational research and discovery; holistic well-being for our campus stakeholders; and public engagement and impact. I can’t wait to make this year another great one for the University of Iowa.”
At 5,178, the 2022 incoming class has 657 more students than last year’s incoming first-year class. About 21% of the class (1,063) are first-generation students, and about 20% (1,061) identify as African American, American Indian, Native Hawaiian or other Pacific Islander, Asian, Latinx/a/o, or two or more ethnicities.
Sarah Hansen, vice president for student life, says the Hawkeye spirit is as vibrant as ever in the newest student cohort.
“I can already tell that the incoming class is going to be an exceptionally engaged class and that they will quickly make their mark on campus,” she says. “They participated in On Iowa! programming in record numbers and are demonstrating their commitment to being a part of the Hawkeye community already. We are so happy they chose us — the UI sense of community is second to none, and we are all here to help them succeed within and beyond the classroom.”
In a speech delivered as part of On Iowa! programming, Cielo Herrera, of Cedar Falls, Iowa, admitted she was nervous yet excited about transitioning to college, and encouraged her fellow first-year classmates to embrace the change: “I urge you all to remain confident in who you are and what you can and will overcome. Change is forever occurring, but may the discomfort form you into something beautiful.”
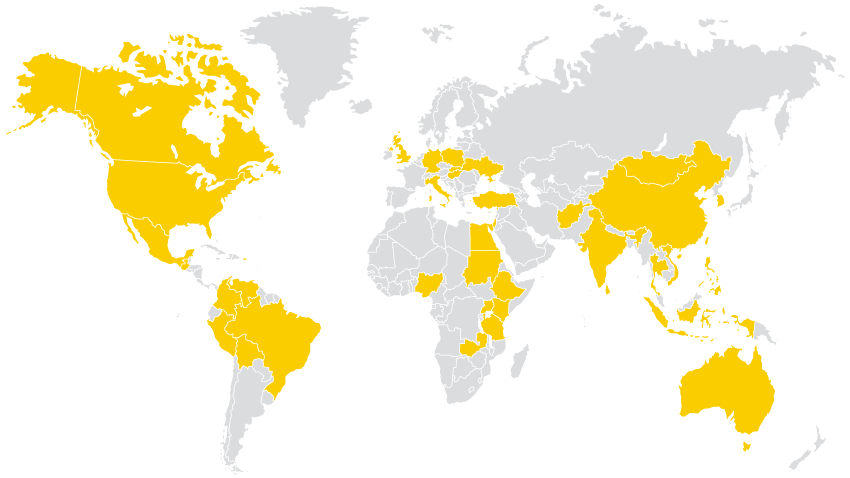
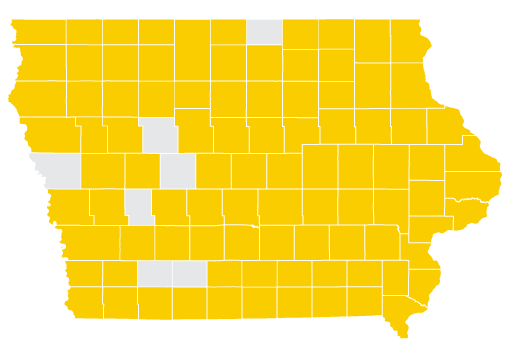
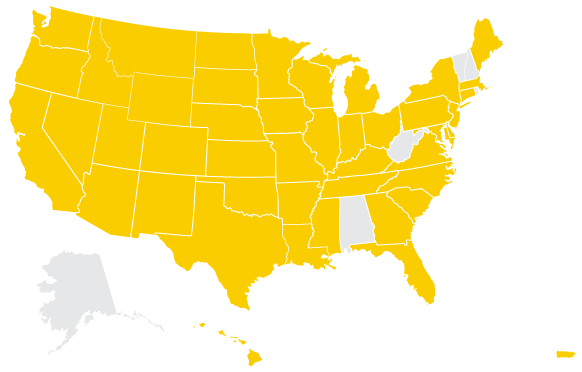
About 54% of the incoming first-year class (2,777) are Iowa residents, and about 1% (55) are international students. The class represents 92 of Iowa’s 99 counties, 45 U.S. states and territories (as well as Washington, D.C., and bases for the U.S. Armed Forces), and 40 countries.
“We know when prospective students see our campus in person, meet our faculty and staff, and experience our downtown, Iowa jumps to the top of their list of schools,” says Brent Gage, associate vice president for enrollment management. “This incoming class is a testament to our university’s collective effort to safely host campus visit programs despite the pandemic.”
This year, 21,973 undergraduates are enrolled at Iowa. About 45% of Iowa’s students identify as male, about 55% as female. Graduate students total 6,156, and professional students total 1,886. Total undergraduate, graduate, and professional enrollment is 30,015 students.
Additionally, Iowa has 1,302 postgraduate scholars (medical residents and postdoctoral students).
This information represents a snapshot of enrollment information from early in the fall 2022 semester and may change with time.
5,178
1,249
2,777
3.82
21 %
20 %
92
45