Putting safety first, and minds at ease

Amy Ward has some advice for those who are thinking twice about a medical procedure at University of Iowa Hospitals & Clinics because they fear infection from the COVID-19 virus.
Don’t worry.
Oh, she understands your concern. She had a procedure scheduled for June, to clear away scar tissue from her trachea to help her breathe and speak with her full voice. And she has an underlying heart condition too, as well as lingering lung issues caused by a fungal infection that left her on life support for two months in 2011. She could suffer serious health issues if she was infected with the virus.
The surgery itself was old hat for Ward. She contracted a water-borne fungal infection while on a kayaking trip, and it caused such extensive lung damage she was intubated for months. Eventually, the intubation tube irritated her trachea so much that thick scar tissue built up around it and made speaking difficult. She needs a surgical procedure every few years to clear away the scar tissue, a procedure that her surgeon, otolaryngologist Henry Hoffman, says is not exactly routine. Anytime a doctor is working in the tight confines of the throat, it could lead to complications that could affect the patient’s ability to breathe or speak, or could damage the spinal cord.

But this was Ward’s 13th surgery with Hoffman since 2012, so the pair knew pretty much what to expect in the operating room. Ward and her husband, Ross Daniels, jokingly refer to the procedure as a “throat-o-rooter.”
“She’s not just a patient, she’s like family to me,” Hoffman says.
Instead, COVID-19 was what was on Ward’s mind as she and Daniels drove to Iowa City from their home in West Des Moines on June 30. They knew COVID-19 patients were in the hospital, and they wondered how could they avoid picking up the virus themselves. What kind of precautions were being taken? Heightening the anxiety was that Daniels’ father had been infected by the virus and died from the disease on May 5.
As soon as they arrived at the hospital, though, their minds were put at ease. The drive-through COVID-19 test, mandatory for all patients before procedures, was safe, orderly, and took only five minutes. Patients, health care providers, and staff members all observed social distancing protocols, whether they were walking in the hallway, discussing their care, or participating in intake interviews.
Everyone wore a mask or a face shield or both, and more importantly, most wore them correctly.
Extensive signage reminded everyone of COVID-19 protocols.
Furniture was arranged to ensure people observed social distancing procedures while they waited, and some hallways were blocked off from use.
Even during the pandemic, you should get the health care you need from your UI Health Care provider. That includes appointments with your primary care provider when you’re not feeling well and necessary appointments for any specialty care you receive.
“The idea of going to a hospital was hugely terrifying for both of us, but once we got there, we saw all the precautions they had put in place and it showed us people were taking this seriously,” says Daniels.
“Our goal is to become one of the safest places in the state of Iowa,” says Suresh Gunasekaran, chief executive officer of UI Hospitals & Clinics and associate vice president for UI Health Care. “We have led the way at putting safety measures in place at scale—face coverings for all who enter our facilities, screenings at all entrances, and much more—but we don’t want to stop there. Testing of all inpatients, regardless of symptoms, will allow us to continue safely caring for all patients’ health care needs.”
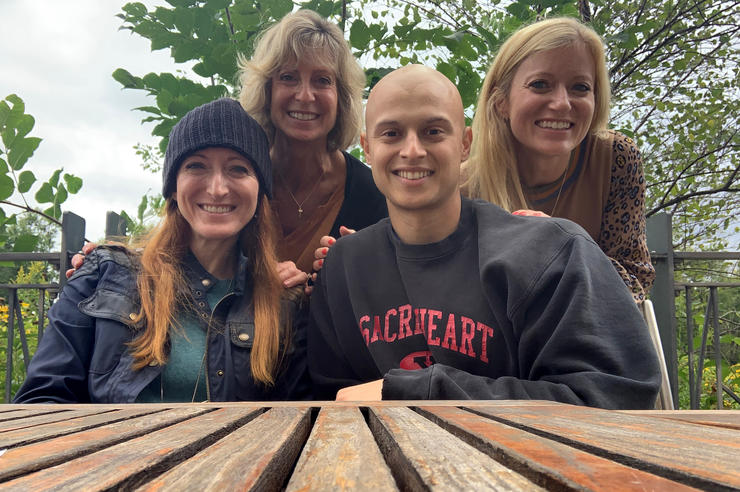
Ward’s latest surgery was successful, and she can breathe easy again for now. Her voice is hale and hearty, so she can talk on the phone, Zoom with family members, and take art classes. She can’t kayak or do anything else in the water anymore due to risk of drowning, but she’s taken up bicycling and rides frequently. She’ll likely need another surgery sometime in the next few years as the scar tissue is likely to build up again, and she and Daniels hope COVID-19 will be history by then. But in the meantime, they know that UI Hospitals & Clinics is a safe place to go if they need to.
“I really don’t have words to express just how much all of the precautions I saw, knowing that there were likely hundreds I did not see, made us feel at ease,” says Daniels. “I am fully convinced that each and every employee, from the executive suite to all other staff, did everything possible to ensure that my wife and I were safe at UI Hospitals & Clinics. This type of leadership comes from the top of an organization but is only successful with the full buy-in from all staff, contractors, everybody. It doesn’t happen on its own.”