Born at 133 days premature, Nash Keen of Ankeny, Iowa, is the new Guinness World Records title holder for the most premature baby.
Story: Taylor Vessel
Photography: Liz Martin and courtesy of the Keen family
Videography: UI Health Care Marketing and Communications
Published: July 23, 2025
It’s an expectant parent’s worst nightmare: Waiting in a hospital room for days surrounded by doctors and nurses, hoping their baby won’t be born too early.
For Randall and Mollie Keen, they needed their baby to be born after midnight on July 5, 2024. If the baby could hold off until then, the expert neonatal team at University of Iowa Health Care Stead Family Children’s Hospital would do everything they could to save their son, Nash.
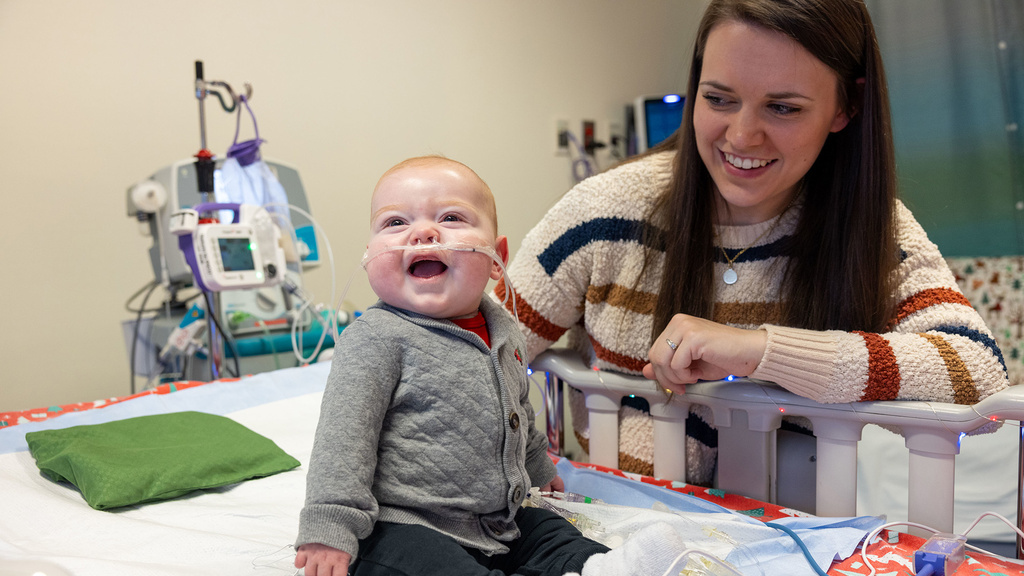
“I never lost hope for Nash,” Mollie says months later, holding a baby who is all giggles.
The family from Ankeny, Iowa, celebrated Nash’s first birthday on July 5, something that seemed nearly impossible a year ago. But Nash — now the Guinness World Records titleholder for most premature baby — is good at beating “impossible” odds.
Remembering McKinley Keen
While Nash’s story is one of triumph, resilience, and a lot of luck, it started with a loss. Less than a year before he was born, his parents, Mollie and Randall, lost a baby girl named McKinley.
“We lost her at just 18 weeks' gestation,” Mollie says. “It was after that when I was diagnosed with an incompetent cervix.”
A condition in which the lower part of the uterus weakens and opens too soon during pregnancy, having an incompetent cervix can lead to preterm birth.
Because Mollie also has polycystic ovary syndrome (PCOS), a disorder that can cause difficulties in getting pregnant, she didn’t know if her dream of having a family would come true. But six months after losing McKinley, the couple discovered Mollie was pregnant again.
The evening after that appointment, Mollie felt some mild cramping, and she rushed to her local emergency room. Mollie was sent home on bed rest, told to “keep in the baby in as long as possible.” She and Randall feared that history would repeat itself.
“We were devastated. We thought we were going through the exact same thing, and we thought we were going to lose this baby,” she says. “At that point, I didn't know what I could do to turn things around.”
Stars align in Iowa City
Mollie posted to an online support group, hoping for an answer. A mom whose baby was currently admitted to the Stead Family Children’s Hospital’s neonatal intensive care unit (NICU) commented on Mollie’s post. She said that the children’s hospital had recently started performing lifesaving measures on babies born at 21 weeks' gestation. This answer was a bit of hope that couldn’t have come at a better time.
“It was 2 a.m. on a Tuesday when I started contracting really heavily,” Mollie says. “We rushed to Iowa City. We checked in. They got us a room. And not long after that, my water ended up breaking.”
This was a major setback, increasing the chance of complications for mom and baby. The care team sprang into action, trying to delay labor. Luckily, Mollie says her contractions subsided for two days. Then, on July 5, just hours after she surpassed the 21-week mark, Mollie’s motherly intuition kicked in once again.
“We never want the parents to lose hope, but many of them are in an unreal situation, so we have to be very honest with them.”
“I just remember feeling a bit off,” she says. “So, I had them check to see how dilated I was and maybe a second later I had a bunch of people in my room.”
One of those people was Malinda Schaefer, MD, PhD, a high-risk obstetrician. Schaefer delivered Nash less than 10 hours after he surpassed the 21-week mark. It was a moment she describes as being part of a new frontier in maternal fetal medicine.
"We want what is best for patients, so we really try to convey that we do not know what the outcomes will be for these extremely premature births. And it is important for parents to understand most survival rates are low, and if babies do survive, they have a very high risk of long-term complications, even at 22 weeks," she says. "Ultimately, it is not me that lives with the outcomes of parents’ decisions, so it is really important to me to have honest and open conversations with parents, so they feel fully informed to make the best decision for them and their family. Patient autonomy is most important to me."
The stars really aligned for Nash as the team was able to quickly provide medicine to support organ development and lower the risk of certain complications. He was also head down, which is better because it was similar to a full-term birth. C-sections and breech deliveries come with a greater risk of complications, Schaefer says.
Thankfully, Nash, she says, “just came out very easily.”
“We were able to deliver in the bed as much as possible and that was yet another advantage for Nash,” Schaefer says. “Once he was out, we were really focused on mom. We try to manage and decrease any blood loss or prevent any hemorrhage."
As Schaefer and others tended to Mollie, they handed off Nash to the care of the NICU team, including neonatologist Amy Stanford, MD, who immediately began to try and answer a question that sounded simple enough.
Was Nash big enough?
“Sometimes babies born at 21 weeks are just too small for even our tiniest breathing tubes and intravenous lines,” Stanford says. “Our NICU team assessed Nash, and I was able to place a breathing tube. Once we had the breathing tube in, his heart rate stabilized, and his oxygen levels were good.”
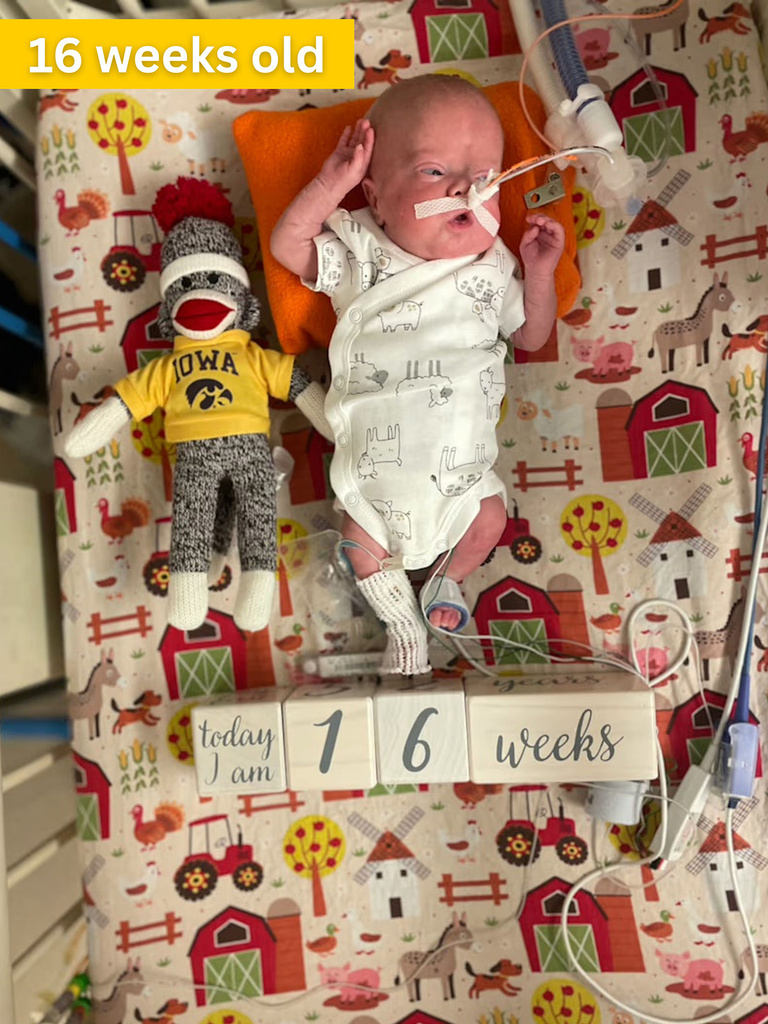
Although he weighed just 10 ounces, Nash was big enough for the smallest equipment. For babies born so early, size can be a huge advantage.
Still, Nash’s chance at surviving was technically nonexistent, because at the time no baby had ever been born so early and survived.
“We never want the parents to lose hope, but many of them are in an unreal situation, so we have to be very honest with them. I would have told his parents, ‘The chance is zero, but I hope I'm wrong and we will do everything we can to help him,’” says Patrick McNamara, MB, BCh, division director of neonatology at Stead Family Children’s Hospital.
Stanford and McNamara both describe Nash as incredibly resilient and, as Stanford says, “he let us do what we needed to do to help him.”
What makes Iowa different
While his parents didn’t know it at the time, there were few places in the world equipped to potentially save Nash. Fortunately, Stead Family Children’s Hospital is one of them.
“Our NICU’s results for babies born at 22 weeks’ gestation are among the best in the world,” says long-time neonatologist Edward Bell, MD. “For this reason, even though 21-week babies like Nash are considered too early to be offered intensive care in most hospitals, we have begun to treat some 21-week babies if their parents wish us to.”
Even with world-class outcomes and expertise, physicians make sure the parents understand all the risks involved with a baby who needs the highest level of care to survive.
It starts with basic support and monitoring of the infant’s organs, which are underdeveloped. Many premature infants face a number of other health challenges, which means treating these babies requires a lot of monitoring and a lot of precision. For McNamara, the difference at Stead Family Children’s Hospital lies in the team’s consistency.
“When another doctor comes on at night to care for the baby, they still provide the same standard of care. We maintain that continuity of care and protocol,” McNamara says.
One such protocol that’s led to their incredible patient outcomes is the use of hemodynamics, a technique that uses ultrasound to precisely assess blood flow and heart function, which allows for highly targeted treatment at the first sign of trouble.
“It allows for us to really fine tune and tailor our therapies,” says Stanford. “For Nash, when he was first born his blood pressure was really low. At first, you might think that means his heart was struggling, but with hemodynamics we were able to check and see that the heart was functioning well, so we adjusted our approach from there.”
Research from the NICU team has shown that hemodynamic care cuts the risk of death or severe brain bleeding in half for very premature babies. Stanford is the second physician to complete Iowa’s unique hemodynamics fellowship program, the first of its kind in the United States. The program focuses entirely on training neonatologists to use hemodynamic care in hopes of providing this unique level of care to babies around the world.
Nash’s NICU rollercoaster
While Stanford and the team were able to quickly stabilize Nash, he faced a lengthy list of health issues in his first few weeks of life. At one point Mollie wrote online, “he's the sickest stable patient they have in the NICU right now.”
“Around the one-month mark, we all began to breathe a little easier,” Stanford says. “While we knew Nash still had a long journey ahead, that was the point when we started to feel more confident that he had a real chance of going home.”

Randall and Mollie Nash had to wait 26 days to hold their son, Nash; now, the couple have a happy, healthy 1-year-old.
As he began to grow, Nash underwent regular blood draws, numerous echocardiograms for his heart conditions, monitoring for neurological issues, and countless medications all with lots of love from his parents.
Mollie and Randall say Nash’s care team really held their hands through the entire process.
“They kept his heart going. They were on top of it every step of the way. They really gave him a fighting chance,” says Randall. “They were really honest with us during the whole journey about what his chances looked like. They made sure we were well-informed and kept us involved in all the decision-making.”
Like any premature baby in the NICU, the care team aims to simulate an environment like that of the mother’s womb to help the baby develop. And like any NICU baby, Nash’s journey wasn’t without challenges. For several nights his vital signs would drop due to his immature lungs and heart. He underwent surgery for a perforated bowel, a procedure that has a 30-40% mortality rate at most hospitals. Through all this, Nash continued to fight.
“We really just follow Nash’s lead. The NICU is a constant roller coaster. He can be doing well for several days and then have one to two bad days in between, but I’m starting to understand that’s part of the journey that most NICU parents go through and that we’re not alone,” Mollie wrote online during Nash’s NICU stay.
Nash’s resilience carried him through months of recovery. After 189 days in the hospital, Nash was finally able to go home in January 2025.
"My ultimate goal for Nash is by the time he's 5 years old, when he goes to kindergarten, no one will know that he was born so early."
What’s next for Nash
Backed by a loving family and expert care team, Nash continues to defy the odds. He’s seen regularly at Stead Family Children’s Hospital and with local specialists in Des Moines, near his hometown.
Stanford continues to follow Nash, focusing on his cardiopulmonary health. The care team recently helped Nash resolve one of his ongoing health issues, chronic pulmonary hypertension. He also has a minor heart defect, which Stanford and the pulmonology team continue to monitor. She says the defect should resolve itself as he gets older. They’re also seeing good progress as they wean him from oxygen.
“My ultimate goal for Nash is by the time he's 5 years old when he goes to kindergarten, no one will know that he was born so early,” Stanford says.
Nash is a bit delayed in reaching the typical baby milestones and isn’t crawling just yet. However, while he was in the NICU, Nash didn’t experience any brain bleeds — something that affects many extremely premature infants — so there’s hope that his cognitive function won’t be affected by his premature birth.
For Stanford and the rest of the NICU team, Nash’s success and positive outcomes come from all the babies who have come before him, like his sister, McKinley.
“Every patient teaches us something, and we use those lessons to improve care for the next,” she says. “Nash’s remarkable outcome reflects the progress we've made by building on the experiences of those patients who came before him.”
Now, his parents say Nash is growing and changing every day, just like any other baby.
“I just hope that Nash realizes just how loved he is and how many people have cheered him on from the very beginning,” Mollie says. “I want him to grow up and be healthy, happy, and confident in who he is. I want him to see his story as a source of strength.”