Multidisciplinary care sends ‘Super Cooper’ home

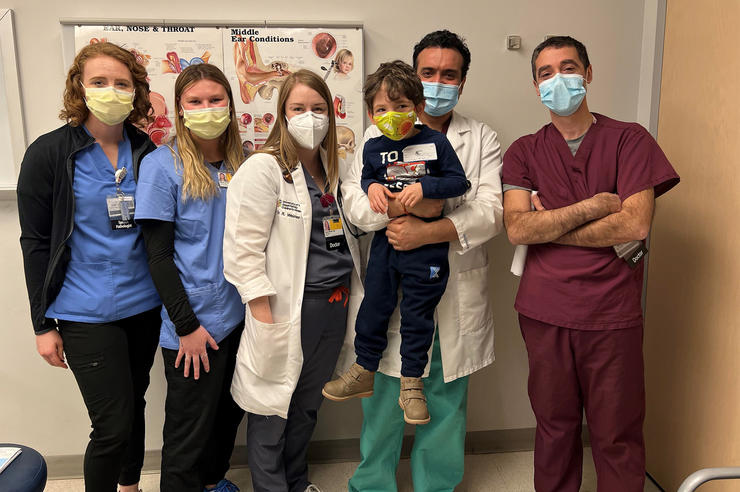
After spending his first 456 days at University of Iowa Stead Family Children’s Hospital, 15-month-old Cooper Schmidt finally got to make his first trip home.
Cooper’s discharge on March 10, 2022, marked the first time he was able to see his Ankeny, Iowa, home—and it was the first time since he was born that his parents, Andrew and Mady Schmidt, have been home, too. The Schmidts built a new home for their growing family in October 2020 but when Cooper was born with a serious kidney disorder two months later, they found an apartment in Iowa City so they could be closer to their son.
“This will be new for all of us,” says Andrew. “This is something we’re all going to experience together.”
Cooper was born with autosomal recessive polycystic kidney disease (ARPKD), a condition that caused development of cysts in his kidneys, making them significantly enlarged and with barely any function. He was placed on dialysis immediately after birth but as he grew his kidneys became even more enlarged, crowding out his lungs and liver. In July 2021 surgeons removed both of his kidneys, giving his other organs room to grow.
As Cooper grew and his health became a bit more stable, he was put on the list for a kidney transplant. A living donor came forward willing to donate a kidney, and on Feb. 7, 2022, Cooper received a new kidney.
Since then, he’s continued to thrive. Two teeth have popped up, he’s becoming more animated, and he’s trying to become more mobile.
“He’s going to be crawling any time now,” Mady says. “It’s been hard at the hospital because he just has his crib, but I can’t wait to see him on our carpet at home.”
Early diagnosis
Mady was 32 weeks pregnant when a routine ultrasound showed Cooper had abnormally large kidneys and very low levels of amniotic fluid. Her doctor in Ames sent her to a Des Moines hospital, who then referred her to UI Hospitals & Clinics and UI Stead Family Children’s Hospital.
“When you have a baby that’s being born with a history of very low amniotic fluid, you worry about the lungs, and you also worry that the kidneys aren’t working well because the kidneys make urine that helps to produce the amniotic fluid,” says Lyndsay Harshman, MD, MS, medical director of the pediatric kidney transplant program.
Most babies with ARPKD don’t have many problems until they are a little older, Harshman says: 70% survive past the newborn period without issues, and 80% of those survive past 10 years old. But by the age of 15, about 40% of patients will be in end-stage kidney disease.
For Cooper, that stage came extremely early.
“This is the kind of renal disease that causes end-stage renal failure and dialysis dependency from birth, so you can assume that doesn’t have a great prognosis to start with,” says Aditya Badheka, MBBS, MS, a pediatric critical care specialist and a member of Cooper’s care team. “But with Cooper, his kidneys weren’t functioning and that led to his lungs being under-developed at birth, so he was placed on a ventilator immediately.”
“If we had gone anywhere else, Cooper wouldn’t be here today. Not just because of his kidney team, but the teams in the neonatal intensive care unit, the pediatric intensive care unit—everyone here is just incredible.”
The need for surgery
As Cooper continued to grow, so did his kidneys – creating even more stress for his lungs and other organs.
“It was very difficult to keep his lungs in good enough shape to keep the oxygen and carbon dioxide levels in the normal range,” Badheka says. “It is extremely hard to dialyze little babies and Cooper’s case was technically challenging. This meant he had more and more fluid on his body from his kidneys not working.”
When Cooper was 7 months old, a pediatric surgery team led by transplant surgeon David Axelrod, MD, and pediatric surgeon Julia Shelton, MD, removed both of his kidneys. Six months later, the surgical team gathered again, along with transplant surgeon Alan Reed, MD, MBA, to transplant an adult kidney donated by a living donor.
The kidney transplant program at University of Iowa Stead Family Children’s Hospital is the only pediatric kidney transplant program in Iowa. Our comprehensive care is coordinated by pediatric specialists dedicated to transplantation and committed to treating each child and family as we would our own. We are approved by the United Network for Organ Sharing (UNOS) to care for children of all ages and have a long track record of outstanding outcomes.
“Cooper’s care has really been a team sport,” Axelrod says. “The surgeons all worked together on both procedures, and Lyndsay and the whole nephrology team have been keeping him healthy on dialysis, getting him to grow. We were very lucky to have someone interested in donating a kidney to someone who wasn’t a family member—getting Cooper a really good, really healthy kidney that has done terrific for him.
“Pretty soon he’ll be running around and doing everything he should be doing,” Axelrod continues. “This is clearly one of the reasons we do this, this is one of these impressive stories of someone in the community wanting to help, of this child being able to have a healthy functioning kidney.”
Cooper’s parents have definitely seen a change in their son since the transplant.
“The first two weeks post-transplant were really rough as he recovered,” Andrew says, “but since then his energy level has just boomed, he has so much energy now. And he’s breathing pretty much on his own; the only time he’s on a ventilator is when he’s sleeping. And we’re going home without any oxygen, which is huge.”
Even with a two-hour drive home, Mady and Andrew are grateful to have a highly specialized pediatric transplant team so close.
“If we had gone anywhere else, Cooper wouldn’t be here today,” Mady says. “Not just because of his kidney team, but the teams in the neonatal intensive care unit, the pediatric intensive care unit—everyone here is just incredible. Knowing we have a nationally recognized pediatric kidney team working with our son is so comforting.”
“Stories like Cooper’s are one of the reasons we do what we do,” says Badheka. “This is such a positive story that gives us all a bit more motivation to keep on doing what we’re doing.”