Making NICU expertise accessible to all Iowans

Everyone expects their pregnancy to go smoothly, so few people can imagine that their baby will be born too early or will have complications needing immediate care. In rural areas, where the closest neonatal intensive care unit may be more than a hundred miles away, having a premature baby is exceptionally frightening when minutes matter most.
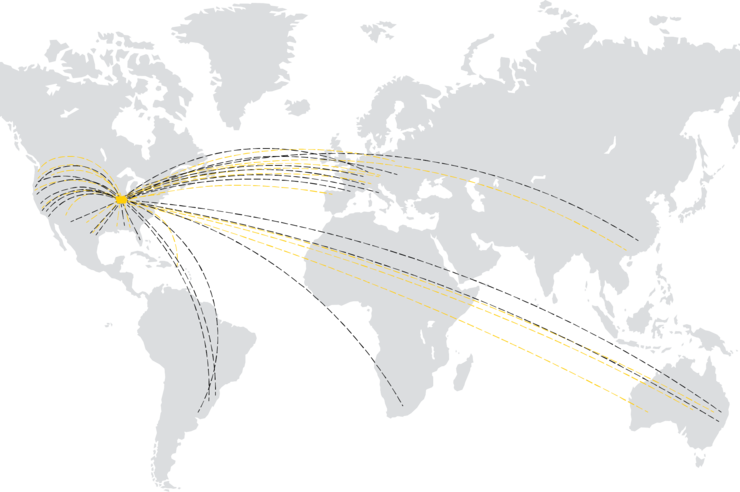
Thankfully, families in Iowa can rest easy knowing when the unimaginable does happen, they now have improved access to the state’s only Level 4 neonatal intensive care unit (NICU) at University of Iowa Stead Family Children’s Hospital through a newly expanded neonatal medical transport service. This is especially important in rural areas where many smaller hospitals no longer have the equipment or staff to deliver even full-term babies.
UI Stead Family Children’s Hospital’s survival rates for babies born as early as 22 weeks is 60%—four times the national average of 15%.
“UI Stead Family Children’s Hospital is unique from other institutions in Iowa in that we have subspecialty expertise—both in the neonatal and pediatric intensive care units—and are able to provide the highest level of care to the most complex and critically ill children,” says Patrick McNamara, vice chair for inpatient acute care and director of neonatology at UI Stead Family Children’s Hospital. “The reason you need a dedicated pediatric transport team is to ensure that critically ill babies and children have a way to be safely transported to specialists for their care.”
The neonatal team at UI Stead Family Children’s Hospital is one of just a handful across the country that will perform life-sustaining efforts for babies born as early as 22 weeks. The hospital’s survival rates for babies born at that mark is about 60%, four times the national average of 15%, McNamara says. That’s why it is so important to provide a service that enables access to that unique expertise across the state, he adds.
Pediatric transport differs from adult transport in that it is based on the concept of a mobile intensive care unit, McNamara says. For extremely preterm infants, such as those born at 22 or 23 weeks’ gestation, or full-term infants who have endured a difficult delivery resulting in potential brain injury it is imperative that the pediatric transport team is dispatched in a timely manner and the highly trained personnel have the necessary equipment to sustain life. This includes equipment such as high frequency ventilators for babies requiring more respiratory support, or state-of-the-art cooling blankets which may minimize the risk of brain injury.
“We have to be able to replicate whatever we do in the neonatal intensive care unit (NICU) as best we can in the transport environment,” he says.

Neonatal Transport
The University of Iowa Stead Family Children’s Hospital transport team specializes in the stabilization and safe transfer of the most critically ill neonates in the state. We provide the highest level of neonatal transport care available.
Learn more.
Pediatric Transport
The pediatric transport program at University of Iowa Stead Family Children’s Hospital provides rapid transfers for sick or injured babies and kids. Our teams specialize in pediatric medicine and focus on delivering a safe, coordinated transition in care.
Learn more.
“We’ve created a team within a team and have made significant investments in provider expertise and system efficiency to ensure that our expertise is available to physicians across the state when they need help caring for a critically ill baby or child with complex needs,” says Regan Giesinger, MD, a neonatologist and medical director of the neonatal transport and hemodynamics programs. “We make it a point to make it easier for other hospitals to immediately access faculty in the NICU, so they have the highest level of advice possible to care for these patients until our transport team arrives and can attend to that patient in person.”
That accessibility comes through mobile neonatal transport equipment and highly skilled neonatologists available both on the phone or video at UI Stead Family Children’s Hospital as well as in the transport unit.
Giesinger says communications have been streamlined with a dedicated telephone number to call for all neonatal and pediatric high-risk transport which provide referring physicians with immediate access to the UI Stead Family Children’s Hospital neonatologist on call. The team works with the attending physician over the phone, combining the expertise of both the attending physician at the community hospital with that of a neonatologist from the state’s highest level NICU.
A future goal is to develop a high-risk maternal transport service, built upon a strong collaboration between high-risk obstetricians from UI Hospitals & Clinics and neonatologists at UI Stead Family Children’s Hospital, McNamara says.
“We know that high-risk babies born at UI Hospitals & Clinics and cared for at UI Stead Family Children’s Hospital are going to have the best chance,” McNamara says, “so if you can move the mother prior to delivery that is best. But we know that’s not always possible. So being able to efficiently transport the babies post-birth and getting them to a place that offers the specialized care they need is extremely important.”